Helpless/Hopeless
Breaking Bad News… For Real
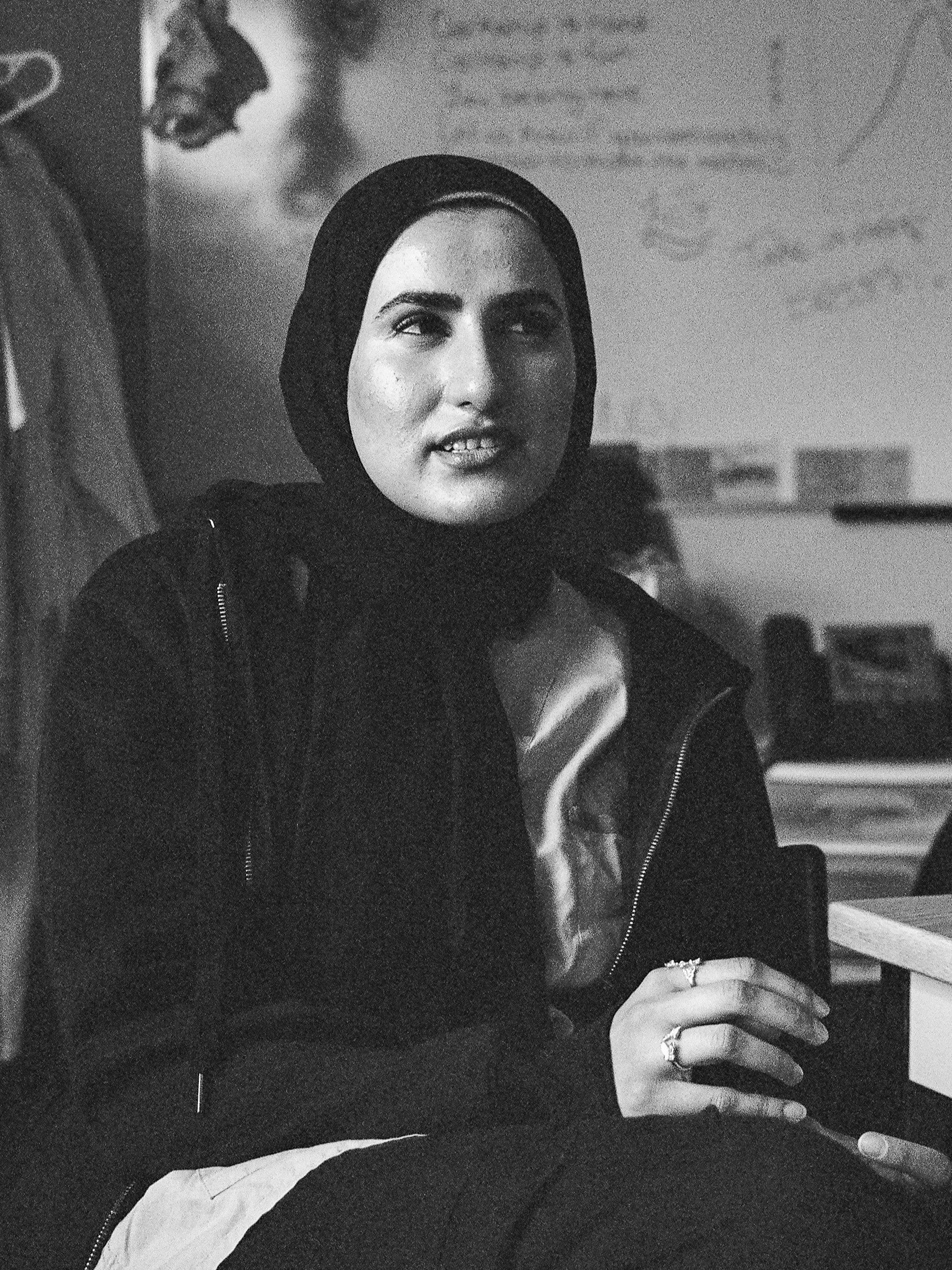
“We’re trying to save lives. Sometimes you just can’t do that.”
This really struck me quite significantly. I was on my rural family medicine rotation, and I was in the emergency department. A woman in her 60s came in, and they were complaining of chest pain with shortness of breath. So, you know, we take a whole history and do an exam, and automatically just based on that we're thinking it’s a pneumothorax. She has that classic presentation. So we're thinking, let's do a CT scan, let's do work up for a pneumothorax and a pulmonary embolism, and some cardiac stuff. Unfortunately, there was no access to a CT so we had to send her somewhere else.
When we get the results for the CT scan, we see that she has huge masses in her lungs, and her kidneys, as well as some that had metastasized to her spine. So, it was quite a shocking revelation, because that's not what we were considering at all. She had a remote cancer history, but it was many, many decades ago it had been treated. She had never had any recurrence. She was routinely being seen by a family doctor for monitoring, and there were never any issues. Overall, she was a pretty healthy patient. But all of a sudden— And for me it was quite a difficult scenario to be in, right? Especially considering this was actually my first emergency shift on rotation. The attending was like, “Oh, well, why don't you break the bad news to her?” So, me as a medical student, going in and being like, “Hey, actually, it's not a pneumothorax and is in fact, cancer.”
It was definitely difficult for me. I truthfully, just couldn't imagine how hard it must be to hear from the patient's point of view. Her husband had actually passed away from cancer about a year ago, and she had taken quite a bit of time to really get over that. And then for her to get that diagnosis of cancer. And because it was metastatic, and because it was lung cancer, she was palliative. I just remember her expression. It was almost like she just went blind. There wasn't any sadness. There wasn't any grief. There wasn't any shock. It was almost an expressionless face. And she just sort of sat there silently, taking it in. As I was going through the options that she had, I talked about palliative care, that we can still try to treat this medically but I didn’t know how successful it would be truthfully, and pain relief. We talked about all these different things. And she just sat there silently, with not a single expression on her face. By the time I was done, she just said, “Okay, that's okay. Thanks for telling me.” And that's all that there was. I left the room, and I could hear her starting to sob in the background. I felt so terrible because it was almost like she was trying to stifle her crying, which made it even harder. It was a wake up to reality because at the end of the day, yes, we're training to be in a profession where we're trying to, as cliche as it is, we’re trying to save lives. Sometimes you just can't do that.
How do you think this is going to impact you and the care that you provide to patients in the future?
I would want to let them know in advance that there are lots of different things that we’re thinking of. So we should have told her that this could be a pulmonary embolism, but could also be something else. I think it would make sense to list out all the things that we're considering and lay the groundwork so the patient’s not completely in shock. I mean, it was a shock for us, it was not something that we were really thinking. It was very, very low on our differential so it wasn't really something that I even mentioned to her but I think even so, I should have said something. We learn about breaking bad news in advanced communication skills but it's one thing to do on an OSCE you on like a OSCE station, but it's completely a different situation when you're doing it in real life, knowing that there are implications for what you say and how you frame things. It's really important that you not only explained what's going on clearly, but make sure you give the patient every single option available. This isn't just something that you can dismiss, this is going to affect them for the rest of their lives.
More Conversations in TCL